The Rhode Island Department of Health (RIDOH) bar chart, below, illustrates how SARS-CoV-2 “delta” became the predominant variant circulating in Rhode Island between July and November, 2021.

See link to larger image of bar chart here: Delta wave RI image pdf
Raw RIDOH data obtained by Rhode Island State Representative Michael Chippendale on covid-19 infections, hospitalizations (with and from covid-19, pooled), and deaths (with and from covid-19, pooled) for these months, stratified by vaccination status, and history of prior covid-19 infection (as a surrogate for “naturally-acquired” immunity), are analyzed in this brief report. Hyperlinks to a downloadable sample RIDOH cover letter (pdf) accompanying the November, 2021 data release to Rep. Chippendale, and the raw July, August, September, October, and November (Excel) data spreadsheets, are provided below.
Cover letter: Chippendale Nov data release email 12.22.21
July, 2021 data: RIDOH July
August, 2021 data: RIDOH Aug
September, 2021 data: RIDOH Sept
October 2021, data: RIDOH Oct
November 2021 data: RIDOH Nov
Definitions, Methods, and Results (in brief)
Definitions for prior infection and breakthrough cases were provided by RIDOH in text typed into the raw Excel spreadsheets. RIDOH defined prior infection history as anyone with a repeat SARS-CoV-2 positive test > 90 days from an initial positive test. A vaccine breakthrough case, per RIDOH, was a Rhode Island resident with SARS-CoV-2 RNA or antigen detected on a respiratory specimen collected ≥ 14 days after completing the primary series of a Food and Drug Administration (FDA)-authorized covid-19 vaccine. RIDOH’s definition of a breakthrough case excluded cases with SARS-CoV-2 RNA or antigen detected on a respiratory specimen collected <45 days before the most recent positive test.
Midpoint estimates for data denominators were made for numbers fully vaccinated, not fully vaccinated, and history of prior infection as of September 15, 2021 from the Rhode Island Department of Health covid-19 data dashboard spreadsheet, U.S. census data (July 1, 2021; n=1,095, 610), and “Covidestim—COVID-19 nowcasting,” a U.S. Centers For Disease Control and Prevention (CDC)-sponsored website run by Harvard, Stanford, and Yale University epidemiologists. These midpoint denominator estimates yielded 690,694 fully vaccinated, 1,095,610 minus 690,694= 404,916 not fully vaccinated, and 1,095,610 X 0.56= 613,542 with a history of prior infection.
Table 1 displays the raw July-November covid-19 infections, hospitalizations, and deaths comparing vaccination status (fully vs. not fully vaccinated) groups, further stratified by history of prior infection. Table 2 depicts the raw rates per 100,000 for covid-19 infections, hospitalizations, and deaths comparing three groups: those fully vaccinated with no prior infection; those not fully vaccinated with no prior infection; and those with prior infection, regardless of vaccination status. Unadjusted risk ratios (with 95% confidence intervals) were also included in Table 2. Those fully vaccinated with no prior infection were the referent group, compared to the two other groups, using raw data from Table 1, and MedCalc software.
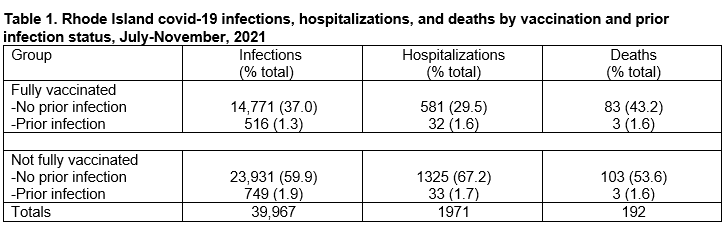
See link to larger pdf image of Table 1 here: Table 1 Delta RI Vax status PI
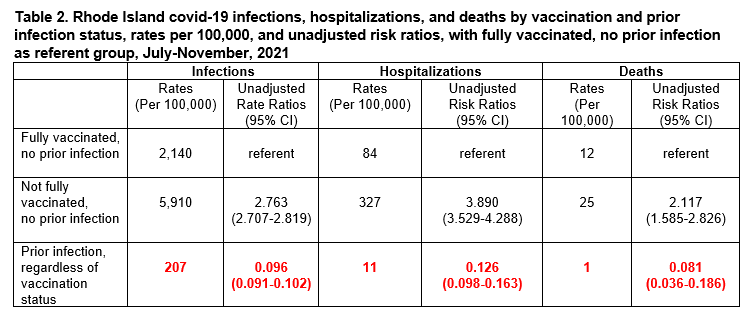
See link to larger pdf image of Table 2 here: Table 2 Delta RI Vax status PI
As can be gleaned from the raw data in Table 1, the fully vaccinated accounted for 38.3% of covid-19 infections, 31.1% of covid-19 hospitalizations, and 44.8% of covid-19 deaths during Rhode Island’s July-November delta wave. Regardless of vaccination status, a disproportionately smaller percentage of those with a history of prior infection contributed to these outcomes: previously infected persons accounted for 3.2% of the infections; 3.3% of the hospitalizations; and 3.1% of the deaths. Adjusting for population pools, Table 2 underscores how irrespective of vaccination status, prior infection conferred dramatically lower relative rates of, and risks for, covid-19 infection, hospitalization, and mortality. Compared to the fully vaccinated, those previously infected had a 10.4-fold lower risk of infection [10.42 (9.80-10.99)], a 7.9-fold lower risk of hospitalization [7.94 (6.13-10.20)], and a 12.3-fold reduced risk of covid-19 mortality [12.35 (5.37-27.78)].
Two large, much more granular age and comorbidity adjusted studies, one from an Israeli health maintenance organization, the other a U.S. medical claims records database analyzed by University of Washington-Seattle investigators, provide rigorous external validation of these unadjusted Rhode Island findings.
The Israeli study of its covid-19 delta period evaluated outcomes June 1 to August 14, 2021, and was published as a preprint August 24, 2021. Analyses were adjusted for age and underlying comorbidities, including obesity, cardiovascular diseases, diabetes, hypertension, chronic kidney disease, cancer and immunosuppressive conditions. Three statistical models were employed. Model 1 (16,125 per group) compared previously infected vs. vaccinated individuals, with matching for time of first event. In this model, the fully vaccinated experienced a 13-fold increased risk for asymptomatic infection (“testing positive”), a 27-fold greater risk for clinical/symptomatic infection, and an 8-fold increased risk for hospitalization. In model 2 (46,035 per group), the previously infected were compared to vaccinated individuals, without matching for time of first event (so previously infected could be infected as far back as the beginning of 2020). Despite this temporal disadvantage for those with prior infection, the fully vaccinated remained at 6-fold increased risk for asymptomatic infection (“testing positive”), 7-fold greater risk for clinical/symptomatic infection, and 6.7-fold increased risk for hospitalization. Model 3 (14,029 per group)–which also did not match for time of event (so, again those previously infected could be infected as far back as the beginning of 2020), compared vaccinated persons, only, with and without a history of prior infection. Covid-19 vaccination of previously SARS-CoV-2 infected persons did not reduce either symptomatic, clinical SARS-CoV-2 infections, or covid-19 hospitalizations.
University of Washington-Seattle investigators published a December 9, 2021 preprint that analyzed claims records from Change Healthcare in a cohort of 8.18 million individuals. They identified 17,881 fully vaccinated patients with SARS-Cov-2 “breakthrough infections” occurring between March 10th and October 14th, 2021. During this observation period, 1121 covid-19 hospitalizations, and 138 covid-19 deaths accrued in the cohort. Prior SARS-CoV-2 infection, in multivariable-adjusted analyses controlling for age, sex, and comorbidities, conferred a 2-fold lower risk [hazard ratio (with 95% confidence interval), 0.49 (0.35-0.69)] for covid-19 hospitalization, and a 4-fold reduced risk [0.24 (0.06-0.98)] for covid-19 mortality, relative to no history of prior infection.
In conclusion, population size-adjusted Rhode Island data make plain how RIDOH’s exclusive, often hectoring comparisons of the covid-19 “fully vaccinated,” versus not fully vaccinated, are clinically meaningless absent appropriate reference to history of prior covid-19 infection. Transparent acknowledgment of this overriding impact of naturally-acquired covid-19 immunity must be demanded of RIDOH by Rhode Islanders given a conservative December 25, 2021 estimate that 71% of the state’s residents had been infected by SARS-CoV-2 at some point during the pandemic.

